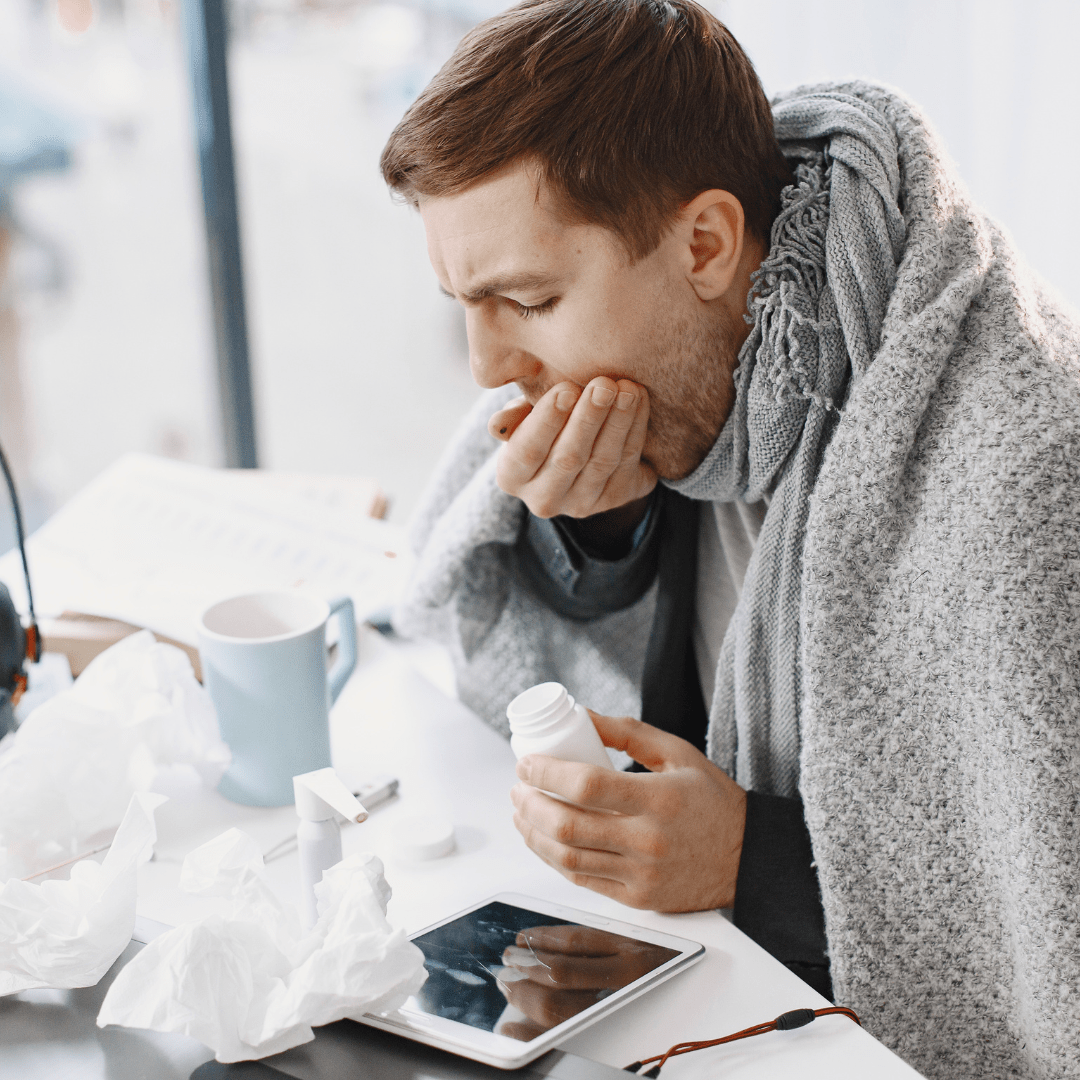
The town doctor, collaborating with the occupational health and prevention service
15 January 2024
The Occupational Health Act of August 2, 2021 enables a town doctor to contribute, in conjunction with the occupational physician, to monitoring employees’ state of health.
The decree that was expected to determine the conditions under which this contribution will be made was published in the Journal Officiel on December 29, 2023, and came into force on December 30, 2023.
Let’s analyze it.
1. WHAT?
Article L4623-1, IV, of the French Labor Code provides for the possibility of a medical practitioner entering into a collaboration agreement with the inter-company occupational health and prevention service.
The terms of this system have now been specified by the decree inserting new articles R4623-41 to R4623-45 into the French Labor Code.
2. WHY?
With the aim of responding to the shortage of occupational physicians in certain parts of the country, this collaboration protocol will contribute to the individual monitoring of the health of employees who are not subject to occupational risks justifying reinforced monitoring.
3. WHO?
A number of protagonists are targeted by this legal apparatus, first and foremost the parties to the protocol: the town doctor, known as the “corresponding medical practitioner“, and the inter-company occupational health and prevention service.
Administrative authorities are also involved, and have been given the task of defining the territories in which the system can be deployed (see 4.).
4. WHERE?
Under the terms of the French Occupational Health Act, collaboration protocols are only authorized in areas where there is an insufficient number or availability of occupational physicians.
The Director General of the local ARS will determine these zones by decree for a maximum period of five years, which may be revised if necessary, in consultation with regional representatives of the French Medical Council (Conseil de l’Ordre des Médecins).
To do so, ARS Director General will be based on a territorial diagnosis of occupational health and with the support of the Dreets (Regional Director for the Economy, Employment, Labor and Solidarity), who will provide him with all the information needed to assess the coverage of companies’ regional occupational medicine needs, after consultation with the Regional Committee for Orientation of Working Conditions (Comité régional d’orientation des conditions de travail).
The assessment of these zones will take into account the situation of inter-company occupational health and prevention services (maximum number of workers monitored, capacity to provide the resources needed to carry out their mission).
5. HOW?
- At least 100 hours of occupational health training
In order to work in the field of worker health monitoring, the corresponding medical practitioner must, as soon as the protocol is signed, have received at least 100 hours of theoretical training, enabling him or her to acquire skills in :
1° knowledge of occupational risks and pathologies and how to prevent them
2° individual monitoring of employee health, including traceability of exposure and health and epidemiological surveillance
3° prevention of loss of employment
This apprenticeship must be issued by a public scientific, cultural and professional establishment, or by one or more Qualiopi-certified organizations, which will attest to its validation.
Exceptionally, when entering into a protocol for the first time, the physician may receive training within one year.
In this case, the text provides for a closer link with the occupational physician until the training validation certificate is issued.
The collaborating practitioner will also be required to spend at least three days in the department before starting work.
- Scope of intervention of the corresponding medical practitioner
At the end of each visit or examination, the corresponding medical practitioner will be able to issue a follow-up certificate to the worker and employer, corresponding to that provided for in Article L4624-1 of the French Labor Code, as part of the information and prevention visit carried out after hiring. If necessary, the corresponding medical practitioner can immediately refer the worker to the occupational physician.
However, it cannot :
- propose individual measures to adapt or change workstations or to reorganize working hours;
- declare an employee unfit for his or her job;
- do not intervene in the reinforced medical monitoring of workers assigned to workplaces presenting particular risks.
- Contents of the collaboration protocol
A model will soon be laid down by decree and must include :
- the procedures for implementing the strengthened link with the occupational physician when the collaborating physician has not obtained it prior to his first intervention in monitoring the state of health of workers;
- the types of visits or medical examinations entrusted to us, within the limits laid down by law;
- the material resources, information and documents required to carry out the mission, made available to the corresponding practitioner by the inter-company occupational health and prevention service;
- how the corresponding medical practitioner uses telehealth tools in the workplace;
- the procedures for inviting workers to medical visits and examinations carried out by the inter-company occupational health and prevention service;
- procedures for referring workers to the occupational physician by the corresponding medical practitioner;
- procedures for access to and input into the occupational health medical file by the corresponding medical practitioner.
For our part, we welcome this legal tool as an initial remedy to the crippling shortage of occupational physicians.
If the collaborating doctor cannot propose accommodations or rule on the unsuitability of workers, his or her practice could help to relieve the – long-awaited – workload of occupational medicine.
But this is only a first step, and we need to go further, quickly.








![Contractual termination vitiated by employee malice [...].](https://www.nmcg.fr/wp-content/uploads/2024/08/Photo-article-85.png)